 The Jeffrey Silver Humanism in Healthcare Research Roundup features summaries of recently published studies on humanism in healthcare.
The Jeffrey Silver Humanism in Healthcare Research Roundup features summaries of recently published studies on humanism in healthcare.
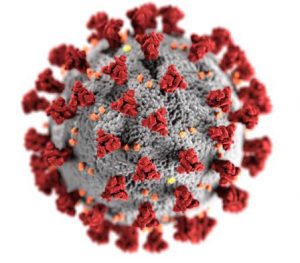
This special edition highlights studies from previous Research Roundup editions that are particularly relevant in the age of COVID-19. As healthcare systems adapt to address the challenges posed by the pandemic, we focus on how we can maintain and strengthen humanism in healthcare during these trying times.
To receive email notification of new studies once per month, enter your information here and select “Jeffrey Silver Research Roundup” from the checkboxes at the bottom. See previous posts in this series.
If you have recommendations for other studies to include in a future special edition, please don’t hesitate to contact us at bkumar@gold-foundation.org.
Self-compassion, trauma, and posttraumatic stress disorder: A systematic review Winders SJ, Murphy O, Looney K, O’Reilly G. Clin Psychol Psychother. 2020 Jan 27. doi: 10.1002/cpp.2429.
Practitioners encountering patients with COVID-19 will likely experience trauma and post-traumatic stress disorder associated with the pandemic. Dr. Winders and colleagues examine how self-compassion can be an intervention to help manage post-traumatic stress disorder.
Post-traumatic stress disorder (PTSD) is an anxiety disorder in which “distinct symptom clusters of re-experiencing, avoidance, and numbing and arousal [persist] for more than one month after trauma.” It is a devastating condition that may be mitigated by self-compassion, in which an individual “treat[s] oneself with the same kindness and compassion as one would treat others in the same situation.” Sarah-Jane Winders and colleagues sought to summarize the relationship between these two concepts by conducting a systematic review. They identified 35 papers; among these, 11 used self-compassion as a form of intervention. These studies support the idea that self-compassion can be helpful in treating PTSD but there were notable limitations. Only two papers compared those with PTSD with those without PTSD, many papers used the now outdated DSM-IV criteria, and there was significant heterogeneity with regards to the trauma, form of intervention, and demographic characteristics of participants. These lead the authors to conclude that more research is needed to explore how exactly self-compassion can mitigate PTSD.
Compassion fatigue in healthcare providers: a systematic review and meta-analysis Cavanagh N, Cockett G, Heinrich C, Doig L, Fiest K, Guichon JR, Page S, Mitchell I, Doig CJ. Nurs Ethics. 2019 Dec 12:969733019889400.
Even before the COVID-19 pandemic, practitioners had been challenged to deliver humanistic care in the face of patient suffering. The additional strain during the pandemic may lead to increased compassion fatigue. Dr. Cavanagh and colleagues look at how this may be related to quality of life and burnout.
Compassion fatigue is the diminished capacity to care as a consequence of repeated exposure to the suffering of patients. It is associated with increased rates of absenteeism, reduced service quality, low levels of efficiency and high attrition rates. Therefore, identifying the prevalence and causes of compassion fatigue is extremely important. Toward those ends, Nicola Cavanagh and colleagues undertook a systematic review and meta-analysis of 71 articles that used the Professional Quality of Life (ProQOL) scale to characterize compassion fatigue. They found that the high scores on the burnout subscale of the ProQOL had the most potentially significant impact on compassion fatigue across studies. Personal factors such as an existing diagnosis of anxiety or depression and prior negative life were also associated with compassion fatigue. Because prevalence is highly variable and its relationship to demographic, personal, and professional variables is inconsistent, the authors stress that approaches to addressing compassion fatigue have to be setting-specific.
Political events and mood among young physicians: a prospective cohort study Free full text Frank E, Nallamothu BK, Zhao Z, Sen S. BMJ. 2019 Dec 9;367:l6322. Dr. Srijan Sen is a Mapping the Landscape grantee.
In addition to being a pandemic, COVID-19 is a global political event. Dr. Frank and colleagues discuss how political events may adversely impact the mental health of young physicians.
Increasing lines of data suggest that young physicians are under a lot of stress and are at increased risk for mental health issues. While there exists a body of research about these stressors within the workplace, less is known about exogenous stressors like dramatic societal and political events. Elena Frank and colleagues used mood data from the Intern Health Study between 2016 and 2018 to investigate how political events impact changes in mood. They identified 9 selected political events and 8 non-political events between 2016 and 2018, and compared the mean mood scores four weeks before these events with mood scores one week after. They found that 6 out of the 9 political events led to statistically significant changes in mood, compared to none in response to nonpolitical events. This study highlights the need to better study how these exogenous factors impact mental health and how we can be more responsive to physician needs to such exogenous factors.
What is clinician presence? A qualitative interview study comparing physician and non-physician insights about practices of human connection Brown-Johnson C, Schwartz R, Maitra A, Haverfield MC, Tierney A, Shaw JG, Zionts DL, Safaeinili N, Thadaney Israni S, Verghese A, Zulman DM. BMJ Open. 2019 Nov 3;9(11):e030831. Dr. Abraham Verghese is a former Gold Foundation Trustee and gave both the 2011 and 2005 Jordan J. Cohen Humanism in Medicine Lecture at the AAMC.
COVID19 is changing the way how patients interact with their healthcare practitioners. However, there remains an urgency to maintain clinician presence while decreasing physical contact and increasing social distancing. Dr. Brown-Johnson and colleagues examine the three requirements of clinician presence.
Clinician presence is a concept that describes a “purposeful practice of awareness, focus, and attention with the intent to understand and connect with individuals and patients.” It’s a powerful concept that contrasts against the depersonalization that is seen in burnout. But what allows a clinician to be present? Cati Brown-Johnson and colleagues explored this in a qualitative study of 10 physicians and 30 non-medical professionals. They found that presence has three requirements: (1) purposeful intention to connect, (2) conscious navigation of time, and (3) awareness of the physical environment. In order to support clinician presence, the authors make several suggestions, including sharing the screen to integrate the electronic health record, integrating caregivers, friends, and family to clinic visits, and incorporating mindfulness in clinical interactions. They conclude by noting that “while challenging to cultivate, this connection offers some of the greatest rewards for practicing physicians.”
Reflecting on shared decision making: a reflection-quantification study Free full text Kunneman M, LaVecchia CM, Singh Ospina N, Abu Dabrh AM, Behnken EM, Wilson P, Branda ME, Hargraves IG, Yost KJ, Frankel RM, Montori VM. Health Expect. 2019 Aug 14. Drs. Marleen Kunneman, Megan Branda, Ian Hargraves, Kathleen Yost, Richard Frankel, and Victor Montori are Mapping the Landscape grantees.
The COVID19 pandemic will require practitioners to improve their ability to engage in shared decision-making. Dr. Kunneman and colleagues examine an instrument that helps to induce a reflective pause when engaging in SDM.
Shared decision-making (SDM) refers to the collaborative nature of clinicians and patients in making decisions about health and care. It is considered an important component of healthcare, but assessing it accurately can be difficult. Marleen Kunneman and colleagues developed a reflection-quantification rubric to determine if SDM can better be measured by prompting patients to reflect before they are asked to produce a numeric rating. To do this, they created two modified versions of CollaboRATE, an SDM self-reported instrument, by adding prompts to reflect either on a particular visit or on a particular decision made during a visit. After testing the three versions of this questionnaire on 107 patients, they pursued further modifications to emphasize “stop-and-think” reflection. In this second study, they distributed a second version of the questionnaire to 212 patients. Overall, they found that that the “stop-and-think” emphasis did not significantly alter the ratings. Still, the authors conclude by noting that “other ways to induce a reflective pause” should be considered when studying SDM in these sorts of challenging settings.
Views of institutional leaders on maintaining humanism in today’s practice Gilligan MC, Osterberg LG, Rider EA, Derse AR, Weil AB, Litzelman DK, Dunne DW, Hafler JP, Plews-Ogan M, Frankel RM, Branch WT Jr. Patient Educ Couns. 2019 Apr 24. pii: S0738-3991(19)30144-2. Drs. Elizabeth Rider, Richard Frankel, and William T. Branch Jr. are Mapping the Landscape Grantees.
Institutional leaders have been challenged by the COVID-19 pandemic to dramatically and rapidly restructure our healthcare systems. Dr. Gilligan examines their perspectives on how to incorporate humanism while engaging in constructive disruption.
Humanism is a core concept of healthcare professionalism, but maintaining humanism in healthcare is challenged by several trends in the United States, including a greater emphasis on clinical productivity, efficiency, and regulation. In order to maintain that humanistic care, institutional leadership is vital, but what are their perspectives and experiences? MaryAnn Gilligan and colleagues examined the views of 32 institutional leaders using interviews and follow-up questionnaires. Although all the interviewed leaders expressed a commitment to humanistic medicine, they noted several technical and adaptive challenges at the institutional level, such as electronic health records, organizational reluctance for change, decreasing reimbursement, and increasing complexity of care. These results help to better characterize larger approaches and solutions to overcome over longer periods of time. Overall, the authors emphasize the need for leaders to “dance on the edge of authority” to take risks and disrupt existing sociopolitical relationships.
Clinician-family communication about patients’ values and preferences in intensive care units. Free full text Scheunemann LP, Ernecoff NC, Buddadhumaruk P, Carson SS, Hough CL, Curtis JR, Anderson WG, Steingrub J, Lo B, Matthay M, Arnold RM, White D. JAMA Intern Med. 2019 Apr 1.
Dr. Robert Arnold is a Mapping The Landscape grantee.
The COVID-19 pandemic challenges practitioners to clearly communicate with family members of those who may be unable to communicate their own values and preferences. Dr. Scheunemann and colleagues highlight the need to discuss these values and preferences so that decisions can be based on the patient’s perceived values and beliefs.
The Intensive Care Unit is a harrowing place in which seriously ill patients largely depend upon the shared decision-making of others, like clinicians and family members, to consider what outcomes and quality of life would be acceptable. But how does this shared decision-making take place? Leslie Scheunemann and colleagues investigated this question by analyzing about 250 clinician-family conference transcripts conducted at 13 intensive care units in 6 U.S. medical centers. They found that 1 in 4 conferences did not contain any information exchange or deliberation about the patient’s values and preferences, and only 1 in 3 addressed physical, cognitive, and social functioning or spirituality. Altogether, only 1 in 12 treatment recommendations by clinicians were based on the patient’s perceived values and beliefs. While daunting, the authors note that this represents an opportunity for interventions to improve clinician communication skills.
The timing of family meetings in the medical intensive care unit. Piscitello GM, Parham WM 3rd, Huber MT, Siegler M, Parker WF. Am J Hosp Palliat Care. 2019 Apr 14.
Dr. Mark Siegler served on the Gold Foundation Research Institute Advisory Board.
Family meetings are essential for guiding the course of treatment while in the ICU for conditions like COVID-19. Dr. Piscitello and colleagues examine patterns in the timing of family meetings and highlight the need to use meetings to learn about patient values rather than solely to negotiate withdrawal of care.
As any patient or healthcare professional who has been through the Medical Intensive Care Unit (MICU) can attest, family meetings are an important aspect of caring for the critically ill. Such meetings help to improve communication, reduce family distress, and align the values of patient’s family with those of the healthcare team. Yet family meetings are often underutilized. To understand this phenomenon, Dr. Gina Piscitello and colleagues looked at the timing of family meetings for 131 patients in the MICU at the University of Chicago. In 46% of cases, there was a family meeting within 72 hours of MICU admission. While this may sound like good news, the timing of these meetings coincided with a 30-fold greater risk of patient death within the subsequent 72 hours. In the remainder of patients, family meetings tended to be held more inconsistently and beyond day 5. This troubling pattern suggests that family meetings are often used to negotiate withdrawal of life support rather than to learn about values. The authors conclude that there are ample opportunities to improve communication skills training for clinicians in the ICU to help maximize the role of family meetings.


